Vulvar Health

OHSU’s Program in Vulvar Health offers expert, compassionate care for disorders of the vulva and vagina and sexual pain. You’ll find:
- The only vulvar and vaginal health specialty clinic in the Pacific Northwest.
- Doctors, researchers and therapists who are leaders in the field.
- An unmatched level of care and support for these often complex conditions.
- Mindfulness and cognitive behavioral therapy for sexual pain.
- Access to clinical trials and research.
Complete, compassionate care
Vulvar and vaginal symptoms can take a toll on your physical, emotional and sexual well-being. Our team will talk with you about all your symptoms and goals to create your care plan. We offer:
- Gynecologists who specialize in vulvar health and who are leaders in research.
- A dermatologist with expertise in vulvar health conditions that affect the skin.
- Referrals to a physical therapist or sex therapist to treat your symptoms if needed.
Our services
We offer:
- Diagnosis and treatment for disorders of the vulva and vagina.
- On-site and off-site physical therapy and rehabilitation of the pelvic floor.
- Extensive experience treating sexual pain.
- Referrals to counseling services for sexual and intimacy issues.
- Surgery for some pain conditions.
Our vulvar health team
-
- Adrienne Bonham, M.D., M.S.
- Accepting new patients
-
- Erin Foster, M.D., Ph.D. (she/her)
- Accepting new patients
-
- Amie Leaverton, M.D.
- Accepting new patients
-
- Catherine M. Leclair, M.D.
- Accepting new patients
-
- Amy L. Stenson, M.D., M.P.H.
- Accepting new patients
Research and clinical trials
We are national leaders in vulvar health research, and have studied vulvar and vaginal conditions for decades. For example:
- One research project resulted in an effective surgical technique for a type of sexual pain called provoked localized vulvodynia.
- To address sexual distress, we developed a group therapy approach using mindfulness and cognitive behavioral therapy.
- We studied painful sex after menopause and learned that lidocaine, a numbing agent, improves pain.
For patients
Call 503-418-4500 to make an appointment.
Location
OHSU Center for Women’s Health, Marquam Hill
Kohler Pavilion, seventh floor
808 S.W. Campus Drive
Portland, OR 97239
Free parking for patients and visitors
Research and clinical trials
At OHSU, many providers are also researchers who strive to turn discoveries into better patient care.
We’re here to listen
Our approach to addressing vulvar pain starts with listening to you.
Our expertise
We treat sexual pain and other disorders of:
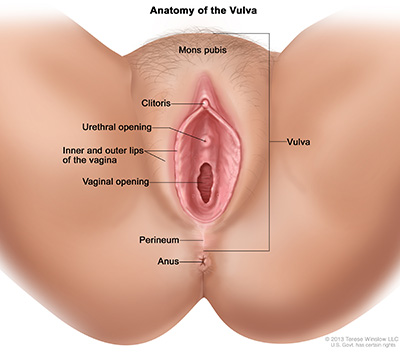
- The vulva. This includes all the external (outside) parts of your genitals (including clitoris and labia).
- The vagina. The tube, sometimes called the birth canal, that leads to the cervix (the opening to the uterus).
- The pelvic floor: The strong muscles that surround and support your bladder, cervix, vagina and uterus. When they contract, the opening to the vagina tightens.
Vaginitis and infections
What is it? Bacterial vaginosis happens when too much of some kinds of bacteria in the vagina upsets the normal mix. It is not an infection, but an imbalance. Bacterial vaginosis is very common in women before menopause.
Symptoms:
- A watery white/gray discharge
- A fishy smell to the discharge
Treatment: Antibiotics, in pill form or vaginal gel.
What is it? Desquamative inflammatory vaginitis is when the skin that lines the vagina becomes swollen.
Symptoms:
- Green, yellow discharge with no odor
- Pain, including with sexual intercourse, irritation and itching
Treatment: Antibiotic creams or steroid creams
What is it? Trichomonas is a common sexually transmitted infection caused by a parasite.
Symptoms:
- Pain, itching or burning in the genitals.
- Discharge, often green-yellow and frothy.
- Pain during sex or when you pee.
Treatment: Antibiotics, in pill form.
What is it? Yeast infections are caused by too much Candida yeast, a type of fungus often present in the vagina. This upsets the normal vaginal balance.
Symptoms:
- Itching and/or redness of the vulva and vagina.
- Thick, white, clumpy discharge that can look like cottage cheese.
- Pain during sex.
- Stinging/burning when you pee.
Treatment: Anti-fungal creams or pills.
Pain disorders
If you have vulvar pain, we can help. We have developed effective treatments for these complex conditions.
What is it? The pelvic floor muscles around your vagina tighten up and clench when something is put into the vagina. It can be painful or impossible to have sex, put in a tampon or have a pelvic exam. Myalgia often develops in response to vulvar pain (see below).
Symptoms:
- An ache, soreness or burning pain in the vulva.
- A feeling that there is a wall or blockage in the vagina.
What is it? Vulvodynia is ongoing skin pain in the vulva with no cause that can be seen. It is thought to be a nerve disorder. The term vulvodynia may also be used for different kinds of vulvar pain.
Symptoms: Long-lasting burning, stinging or rawness of the vulva.
What is it? This is pain at the vagina’s entry, called the vestibule. It is caused by touch or pressure from, for instance, putting in a tampon or trying to have sex with vaginal penetration.
Symptoms:
- Severe pain when the vaginal opening is touched.
- Tenderness to any pressure at the entrance to the vagina.
- Skin redness.
Lidocaine: This numbing liquid lessens nerve pain when applied to the vulva just before sex.
Physical therapy: This helps with the muscle pain and clenching that often comes with vulvar skin pain.
Biofeedback: We place electronic sensors on or in your body to measure the activity of your pelvic muscles. The sensors are connected to a computer where we see or hear your muscle movements as a flash of light, a graph, or a sound. The feedback on the screen changes as your muscles relax or tighten. These images or sounds give you a sense of how your muscles move and help you learn to control them.
Dilator therapy: At home, you practice putting smooth tampon-shaped objects of different sizes into your vagina. This helps you learn to relax your pelvic floor muscles.
Professional counseling: Sex therapists at the Center for Women’s Health can help you with the sadness and guilt that may come with sexual pain disorders. We can also help you and your partner talk about sexual problems.
Surgery: We have developed a procedure for vestibulodynia that removes surface tenderness. About 85% of patients who have the surgery have significantly less pain. The procedure can be done in one day, including in clinic with local anesthetic.
Vulvar skin disorders
What is it? Contact dermatitis is pain and itching of the vulva caused by irritants like soaps, fabrics or perfumes.
Symptoms: Extreme itching, rawness, stinging, burning and pain.
Treatment: Use only warm water and gentle cleansers to wash your vulva. To prevent burning and itching, avoid:
- Scented soaps, perfumes, detergents, bubble baths.
- Fabric softener.
- Sprays and douches.
- Scented or deodorized menstrual pads or tampons.
- Fabrics that cause irritation. Try 100% cotton underwear.
What is it? Lichen simplex chronicus is damage to the skin of the vulva because of chronic scratching.
Symptoms: Thickened, rough and sometimes dark skin patches.
Treatment: Steroid ointments work well for most women.
What is it? Lichen planus is inflammation of the skin of the vagina and vulva. It may be triggered by your immune system.
Symptoms:
- Vaginal discharge,
- Pain, burning and itching.
- Sometimes there are red painful areas, called erosions, on the vulva.
Treatment: It can be managed with steroid ointments.
What is it? Lichen sclerosus is a long-term skin disorder that produces patches of white, abnormally thin skin.
Symptoms:
- Small, white areas on the vulva that might look crinkly or transparent.
- Intense itching, pain, burning and irritation.
- Over time, skin changes and scars can make sex, peeing and bowel movements difficult.
Treatment: There is no cure, but symptoms can be controlled with steroid ointment. The goal is to get rid of symptoms and to prevent scars and skin damage.
What is it? Abnormal cells develop in the top layer of the skin that covers the vulva. Over time, these cells may become cancerous.
Symptoms:
- Itching
- Pain
- Discomfort or pain during sex
- Patches of red, white, gray or brown skin on the vulva
- Some women have no symptoms
Treatment: This depends on how deeply the abnormal cells go into skin layers. It might include:
- Close monitoring
- Chemotherapy cream on the affected skin
- Surgery
Bartholin gland disorders
The Bartholin glands are found on either side of the opening to the vagina. They produce fluid that keeps the vagina moist.
What is it? If the Bartholin glands get blocked, fluid backs up and forms a cyst (a fluid-filled lump).
Symptoms: You may notice a small lump or feel discomfort, pain or pressure during sex.
Treatment: The cyst can be drained. If you keep getting cysts, surgery can help.
What is it? If the Bartholin glands become infected with bacteria, you may get an abscess.
Symptoms: A painful lump under the skin that might be warm to the touch. It can hurt to walk, sit or have sex.
Treatment might include:
- Antibiotics
- Draining the abscess
- Surgery for frequent abscesses
Learn more
- National Vulvodynia Association
- Disorders of the Vulva, American College of Obstetricians and Gynecologists
- Sexually Transmitted Diseases, Centers for Disease Control and Prevention
- International Society for the Study of Vulvovaginal Disease