Pancreatic Cancer Treatment

Knight Cancer Institute experts work together to give you tailored care for pancreatic cancer. We know how important it is to provide the right treatments in the right order.
Our care includes:
- World-class surgeons who make surgery possible for more patients
- Compassionate providers to help you live the best and longest life possible
- Advanced chemotherapy and radiation therapy
- Specialists who pool their knowledge to review results and plan treatment
- Clinical trials and advanced therapies in collaboration with the Brenden-Colson Center for Pancreatic Care
This page focuses on care for exocrine pancreatic cancer. We also treat pancreatic neuroendocrine tumors, or NETs.
Treatment overview
Treatment goals
We have patients who are long-term survivors of pancreatic cancer. For most patients, though, a cure isn’t possible because the cancer spread too far.
Even so, you may enjoy years or months of meaningful life. You may set goals such as taking a special trip or attending a loved one’s wedding or graduation.
At the Knight Cancer Institute, your goals become our goals. Your team will be devoted to extending and improving your life regardless of your long-term outlook.

Whether your tumor can be removed in surgery will guide many decisions. This is important because removing all of the tumor, combined with other treatments, is the only path to a cure.
Based on your diagnosis, your tumor will be described one of these ways:
- Resectable: Removable with surgery
- Borderline resectable: May be removable with surgery
- Locally advanced: May or may not be removable with surgery
- Unresectable: Not removable with surgery
Resectable or borderline resectable
You may have chemotherapy or chemoradiation (a combination of chemotherapy and radiation therapy) to shrink the tumor before surgery. This helps increase the chance that surgeons can remove all the cancer.
If you have surgery, you may have more treatments to destroy any remaining cancer cells. This lowers the chances of cancer coming back.
Locally advanced
You will get chemotherapy and maybe radiation therapy. Some patients with locally advanced pancreatic cancer have surgery.
Unresectable
Your treatment plan may include:
- Chemotherapy and radiation therapy to slow cancer and control symptoms
- A procedure to keep your bile duct open
- Palliative care to control pain and ease symptoms
- A clinical trial with a new therapy that may lengthen and improve your life
Chemotherapy for pancreatic cancer
Chemotherapy delivers cancer drugs in an IV, in a process called infusion. Depending on the drugs, patients may have an infusion every week or every other week. Each infusion takes several hours.
Chemo can come with big side effects. Still, research shows that it helps people with pancreatic cancer live longer and more comfortably.
Our medical oncologists (doctors who are experts in cancer medications):
- Use the most advanced drugs and infusion techniques
- Tailor drugs to each patient’s needs
- Provide chemotherapy in a way that offers the best outcome, for example by making sure a patient still qualifies for clinical trials
When chemotherapy is given
Doctors decide when to offer chemotherapy based on each patient’s needs.
Before surgery (neoadjuvant):
- Chemotherapy can destroy cancer cells, helping make sure surgery removes more cancer.
- It can shrink some borderline tumors enough to be removed with surgery.
- It can attack tiny clusters of cancer cells that doctors can’t see, making surgery more successful.
- It can help doctors see if chemotherapy fights the cancer. This helps avoid putting people through major surgery that won’t help.
After surgery (adjuvant): Chemotherapy after surgery can kill cancer cells circulating nearly anywhere in the body, increasing chances of living longer.
If you’re not having surgery: Some patients receive only chemotherapy or radiation therapy.
Radiation therapy for pancreatic cancer
Radiation therapy uses beams of energy to destroy cancer cells. For pancreatic cancer, radiation therapy is external, meaning you get it from a machine outside your body.
The Knight Cancer Institute uses the most precise methods. We are also one of the nation’s top cancer centers to offer radiation therapy during surgery.
This is the most common type. It delivers energy beams in the exact shape of the tumor. This allows a higher dose while protecting healthy tissue. It is often combined with chemotherapy. Patients get treatments five days a week for two to six weeks.
This is a type of 3D CRT. It allows the doctor to deliver different doses from different angles to different parts of the tumor. Parts with more cancer cells can get higher doses, for example. This treatment is often combined with chemotherapy. Patients get treatments five days a week for two to six weeks.
This type delivers high, precise doses of radiation to the tumor in fewer treatments. Usually, patients get treatments once a day for less than a week.
This type is given during surgery. It lets us use a high dose of radiation precisely targeted at the area that needs treatment. It delivers seven to 10 days’ worth of therapy in one dose.
When radiation therapy is given
Studies show that patients with pancreatic cancer do best when they receive radiation therapy before or after surgery, not both. Radiation during surgery, however, can be combined with either.
Before surgery (neoadjuvant): Radiation therapy might be combined with chemotherapy to shrink a tumor before surgery.
During surgery: Interoperative radiation therapy can be precisely delivered in a large dose.
After surgery (adjuvant): Radiation therapy can kill any cancer cells left after surgery, improving chances of living longer.
If you’re not having surgery: You might have radiation therapy to slow the cancer’s growth and to control symptoms.
Pancreatic cancer surgery
We provide the highest level of surgical care and make surgery possible for as many patients as possible. Our surgeons do nearly 100 pancreatic surgeries each year.
- Your care team will make sure you are as healthy as possible for surgery.
- Your pancreatic surgeons and vascular surgeons will work together to remove cancer and repair blood vessels.
- We offer minimally invasive and robotic-assisted surgery for patients who qualify.
- We offer complete follow-up services to keep you healthy after surgery.
Preparing for pancreatic surgery
Proper nutrition and activity in the weeks before surgery can lower the risk of complications and speed recovery.
If you are having surgery, first you will see:
- A cancer dietitian, to help you improve your diet and activity
- A physical therapist, to help improve your fitness
- A mental health counselor, if needed, for you and your family
- Staff in our pre-operative medicine clinic, to make sure you are ready for surgery for the best results
- Our perioperative team, to make sure the day of surgery is as safe and comfortable as possible.
The Whipple procedure
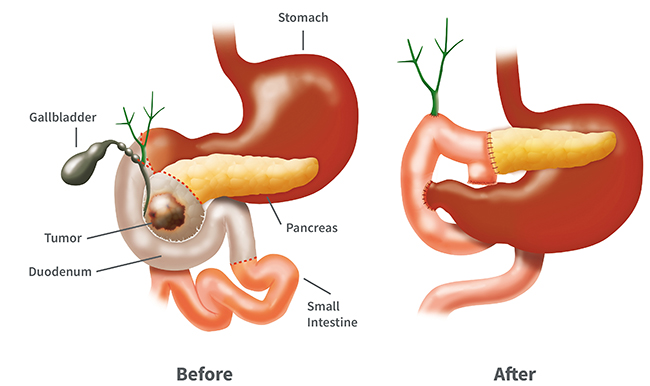
The Whipple procedure is the most common surgery to remove pancreatic cancer. It’s named after Allen Whipple, the first American doctor to do it. Because it has a higher risk of complications and requires a long recovery, our doctors advise some patients against it.
How it’s done: The surgeon removes most of the pancreas. The surgeon may also remove the duodenum (top of the small intestine), gallbladder, part of the bile duct and part of the stomach. The surgeon reconnects the remaining pancreas, bile duct and small intestine so you can digest food. The surgeon also reattaches the stomach and small intestine to restore your digestive tract.
Why experience matters: This surgery is very complex. Skilled surgeons can greatly lower risk. Knight surgeons do dozens of these surgeries a year. We are consistently named as one of the best hospitals in the country for gastrointestinal surgery.
Vascular expertise: Our pancreatic surgeons work with expert vascular surgeons to repair and rebuild blood vessels damaged by or surrounded by cancer. This makes surgery possible for patients who didn’t qualify in the past.
Pancreas anatomy
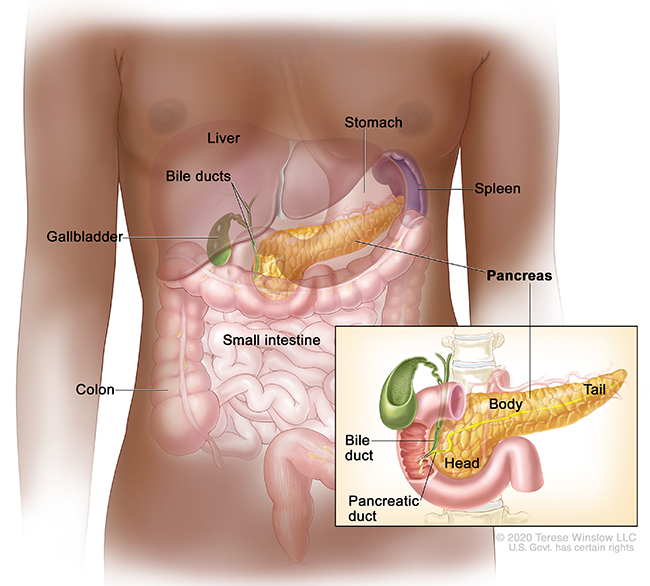
Other pancreatic cancer surgeries
Most pancreatic tumors form in the head of the pancreas. This surgery is used for cancer in the body or tail. The body and tail are removed, along with the spleen. Sometimes part of the stomach and an adrenal gland are removed.
When a tumor is in the tail of the pancreas, the surgeon can remove it and sometimes part of the body of the pancreas and the spleen. This surgery may be done using small incisions and tiny instruments.
This surgery is rarely done for pancreatic cancer. Usually, it’s done for precancerous conditions. Surgeons take out the pancreas, gallbladder, spleen and nearby lymph nodes. They also remove parts of the stomach, small intestine and bile duct.
Some people develop a pancreas condition called intraductal papillary mucinous neoplasm. Because some people with this condition will develop pancreatic cancer, surgeons may recommend a preventive Whipple procedure, total pancreatectomy or other surgery.
Sometimes a surgeon starts surgery only to find that the cancer is too advanced for removal. To ease symptoms, the surgeon may:
- Cut nerves or inject alcohol into them to stop pain
- Attach the small intestine to the bile duct to bypass the pancreas, preventing cancer from blocking the duct
- Attach the stomach lower on the small intestine, which can avoid cancer blocking the top of the small intestine
Follow-up care
After surgery, many people need:
- Enzyme pills for digestion
- Insulin shots in the hospital to control blood sugar
After you leave the hospital, you can continue care with a cancer dietitian or an endocrinologist, a doctor who is an expert in hormones.
Clinical trials
As Oregon’s only academic health center, OHSU is a leader in researching new ways to prevent, detect, treat and manage pancreatic cancer. We offer clinical trials to test therapies for every stage of illness. Your care team will work to find a trial for you.
Learn more
- OHSU Brenden-Colson Center for Pancreatic Care
- Treating Pancreatic Cancer, American Cancer Society
- Pancreatic Cancer Treatment, National Cancer Institute
- Treatment, Pancreatic Cancer Action Network
- Pancreatic Neuroendocrine Tumors (Islet Cell Tumors) Treatment, National Cancer Institute
For patients
Call 503-494-7999 to:
- Make an appointment
- Seek a second opinion
- Ask questions
Location
Knight Cancer Institute, South Waterfront
Center for Health & Healing, Building 2
3485 S. Bond Ave.
Portland, OR 97239
Free parking for patients and visitors
Refer a patient
- Refer your patient to OHSU.
- Call 503-494-4567 to seek provider-to-provider advice.
Cancer clinical trials
Clinical trials allow patients to try a new test or treatment.
Read more
Learn more about OHSU Knight Cancer Institute treatments:
- Surgery
- Chemotherapy/medical oncology
- Radiation therapy
- Immunotherapy
- CAR T-cell therapy
- Targeted therapy
Find other pancreas care at OHSU.