Capturing photoreceptor dysfunction
In the realm of eye care, new technology is constantly redefining the approach to diagnosis, treatment and management. Recently, a new imaging technique called OCT optoretinography (ORG) demonstrated its potential for revealing photoreceptor dysfunction in the macula.
The technique is a new way of using optical coherence tomography (OCT), which was co-developed by Lasker Award-winning Casey Eye Institute faculty member David Huang, M.D., Ph.D., who directs Casey’s Center for Ophthalmic Optics and Lasers (COOL lab).
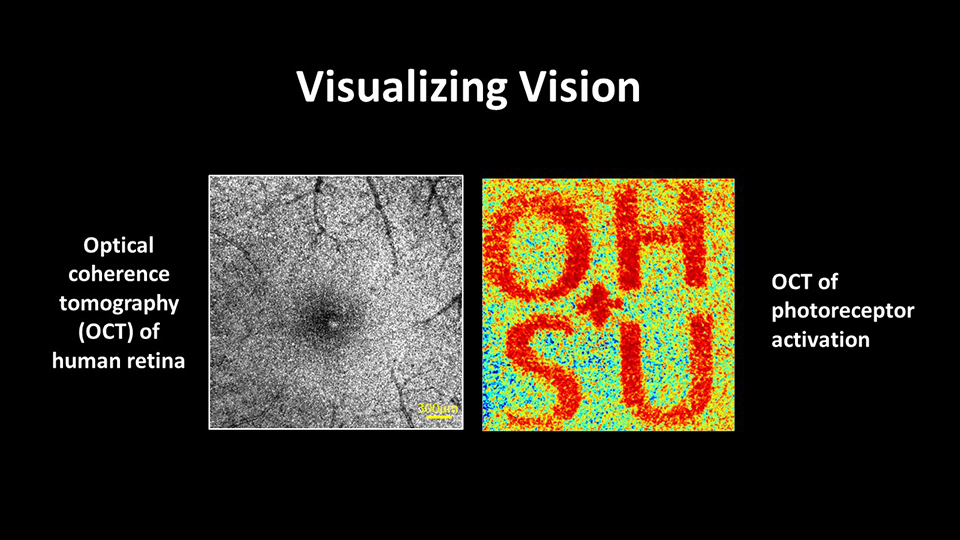
Casey Eye Institute researcher Siyu Chen, Ph.D., who works in the COOL lab, has been instrumental in this advance. He produced the graphic shown above, demonstrating how ORG technology reveals photoreceptor activation compared to a regular OCT image, where the letters “OHSU” are not visible as they are with ORG.
The development is exciting because it shows which retinal cells are actually working. “These ORG images are a surrogate marker for visual perception,” says Dr. Chen. “Loss of ORG response corresponds to vision loss. That is important information for the clinical trials of the future as we try to slow or stop the progression of retinal diseases. Preservation of ORG response in patients taking a trial drug suggests that drug is safe and effective.”
How ORG works
ORG works by measuring how the light-sensitive cells in the retina, called photoreceptors, respond to stimuli. When a photoreceptor is stimulated by light, its shape and reflectivity change slightly. ORG detects these changes and creates a map of the retina that show areas with functional photoreceptors in contrast to areas with dysfunctional photoreceptors. This gives researchers unique insight into how well the cells are actually functioning, as opposed to their structural appearance, which may not tell the whole story.
An evolving technique
ORG was first demonstrated more than a decade ago. The initial application used adaptive optics to look at and track the function of single photoreceptors. However, the field of view was less than 1 mm square. ”It’s not possible to monitor disease with such a small field of view,” says Dr. Chen. “It takes too long to look at the critical areas, and you might miss something.”
The COOL lab uses an efficient split-spectrum amplitude-decorrelation optoretinogram (SSADOR) technique that holds promise for significantly expanding the field of view. Currently, the lab can create a 1x3 mm scan and an unprecedented 3x3 mm montage. They are working to expand the viewing field to a single scan of 3x3 mm and a montage of 6x6mm. This would cover the whole macula – the part of the retina that is responsible for high-resolution vision used in critical tasks such as reading, which is damaged in age-related macular degeneration.
A larger ORG image will give retinal specialists much more information on a patient’s retinal disease. Today, many retinal diseases are not clinically apparent until the disease process is fairly advanced and the patient has irreversible vision loss. ORG has the potential to play a critical role in monitoring disease progression and assessing response to novel therapies, particularly in “dry” age-related macular degeneration and inherited retinal diseases. It holds enormous promise for slowing progression of vision-robbing diseases through early detection, understanding and treatment development.
Comparative advantages
While similar work is being conducted using adaptive optics, it is typically expensive, complex, and restricted to a smaller viewing area. Dr. Chen's work with ORG stands out for its simplicity, clinical readiness and larger field of view.
Collaboration for faster innovation
Collaboration with ophthalmologists and other vision researchers is vital to this innovation. Dr. Chen emphasizes the role of shared resources, clinical collaboration and the expertise of faculty members at Casey Eye Institute in developing ORG. Working with faculty members and clinical collaborators like Mark Pennesi, M.D., Ph.D., the COOL lab has been able to build machines quickly and conduct patient studies based on disease genotypes and phenotypes.
A glimpse into the future
Dr. Chen is optimistic about ORG's potential as a biomarker for visual function in clinical trials. Current clinical trials of dry age-related macular degeneration often use fundus autofluorescence to map areas of geographic atrophy – areas of advanced damage where photoreceptors are completely gone.
By mapping function, ORG could provide a precise way to assess the effectiveness of therapies in earlier stages of the disease. Subjective tests to map visual function, such as perimetry or visual field testing, are time-consuming, tedious, and often unreliable. By contrast, ORG is an objective test providing precise, detailed and reliable results.
When clinical studies are complete, the team expects ORG to be easily integrated into existing commercial instruments. “The technology can be scaled to work in a broader clinical area,” says Dr. Chen.
The advent of ORG opens up new possibilities in ophthalmic imaging, promising a future where the early detection and monitoring of retinal diseases become seamlessly integrated into clinical practice. It could provide a powerful tool to speed the development of treatment for early macular degeneration and save the sight of millions.